For the first time, previously unusable chemotherapy drugs reached brain tumors in humans after a cutting-edge procedure by a Northwestern University team.
Doctors achieved the breakthrough with an innovative mix of ultrasound and microbubbles that opened the blood-brain barrier to allow the drugs to pass through.
“This is a starting point to open the doors for the 95% of drugs that are usually not considered for treating brain diseases,” co-lead investigator Dr. Adam Sonabend told the Tribune Tuesday.
The Northwestern team released a report on the use of the procedure to treat 17 patients with glioblastoma, the most common and malignant form of brain cancer that has often been viewed as incurable. The treatment led to a four- to sixfold increase in drug concentrations in the patients’ brains, the researchers determined.
“We were able to get concentrations that are meaningful, that are compatible with the ranges that you would expect to be necessary to kill tumor cells,” Sonabend said.
To conduct the procedure, the Northwestern team implanted small, ultrasonic devices into patients’ skulls after removing tumors from their brains. Then, as microbubbles and chemotherapy medications were intravenously injected, the devices emitted ultrasound to open the blood-brain barrier.
The “sonication” agitates the microbubbles to open the blood-brain barrier, allowing the drugs to pass from the bloodstream, into the brain and more directly to the tumors.
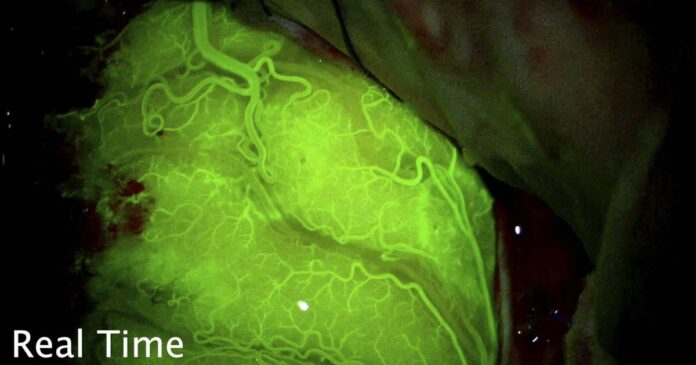
Neurosurgeon Sonabend knew it had worked when his patients’ brains glowed bright green.
The blood-brain barrier that blocks many drugs used to treat cancer also blocks radiant fluorescein dye, Sonabend said. When he injected the dye while using the ultrasound procedure, the dye appeared first in the patients’ blood vessels, video shows.
But then the dye passed the obstinate blood-brain barrier to spread into the brain. The patients’ brains shone under their skulls like glow sticks.
“This project is unique because it opens completely new avenues to drugs that have not been used,” said Dr. Roger Stupp, chief of neuro-oncology at Northwestern University Feinberg School of Medicine, who also helped lead the project. “This is the first trial that has taken it to the next level with chemotherapy drugs that you would normally not use for brain tumors.”
Glioblastoma affects around 14,000 people each year in the United States, Stupp said. The disease is typically fatal within two years of diagnosis, he said.
Doctors haven’t had many options treating the disease, Sonabend said. They could operate to remove the bulk of the tumor and use a limited set of less effective drug therapies to improve patient outlooks, but “universally, these tumors always come back,” he said.
In glioblastoma patients, cancer cells scattered throughout the brain surrounding a tumor inevitably linger after tumors are removed in surgery, Sonabend said. They have long been impossible to get to, in large part because the blood-brain barrier blocks drugs typically used to fight cancer from reaching them.
When left behind, those leftover cancer cells grow. The Northwestern research shows medicines capable of treating those leftover cancer cells can reach the brain.
Patients in the trial got up to six cycles of treatment using the implanted ultrasound device, which was created by French biotech company Carthera. The ultrasound is used for four and a half minutes, after which patients receive chemotherapy, Stupp said.
Patients remain awake for the whole procedure. It takes under two hours, and the medical team’s results show the treatment is safe and the blood-brain barrier is quickly restored, Stupp said. The ultrasound device remains implanted in patients’ skulls under their skin, allowing for it to be easily used throughout the treatment rounds.
Some patients expected chemotherapy side effects, Sonabend said. But the patients go home a few hours after the treatment, he added.
“It’s remarkable how well people have tolerated this,” Sonabend said.
Rod Boyer of Terre Haute, Indiana, felt like he didn’t have any promising treatment options when he volunteered for the experimental procedure. He already had a golf-ball sized tumor removed in July before another tumor surfaced months later, the glioblastoma patient said.
“It was about my only choice,” the retired sheet-metal welder said.
Doctors implanted the ultrasound device into Boyer’s skull in January after removing his second tumor. He’s since undergone five rounds of the ultrasonic chemotherapy treatment.
During the treatment period, he’s dealt with the aches and pains many people undergoing chemotherapy experience, he said. But he’s also felt “a lot better” since his visits to Northwestern began, he said.
The procedure itself doesn’t hurt, Boyer said, though he can hear the microbubbles inside his head as the ultrasound device is working.
“It’s like a tick-tick-tick, bubbling, popping,” he said. “But it’s truly not that bad.”
The innovative procedure has given the 60-year-old hope as he faces a cancer that he knows has been described as “incurable.”
“I hope they’re on to something good,” he said.
Sonabend certainly thinks the medical team is, in fact, onto something good. Because there isn’t a large market for brain cancer drugs, few new drugs ever come out for glioblastoma patients, he noted. The potential to apply drugs used to treat other cancers could be game-changing in treating the disease.
And the possibilities extend beyond glioblastoma, Stupp said. The procedure’s ability to bypass the blood-brain barrier could be used to treat Parkinson’s, Alzehimer’s and other brain diseases, he said.
“It opens new opportunities in treating brain disease at large,” Stupp said.
He credited Northwestern’s spirit of collaboration, especially at the Lou and Jean Malnati Brain Tumor Institute with enabling the breakthrough, as well as funding from philanthropists and the National Institutes of Health.
Still, the success is a first step, Stupp noted.
Doctors now need to prove the treatment can help patients live longer and determine which drugs work best with the procedure. He’s optimistic as the trials move ahead.
“It’s unique. It’s a different concept,” he said.