Researchers say they’ve located a “kill switch” that can trigger the death of cancer cells.
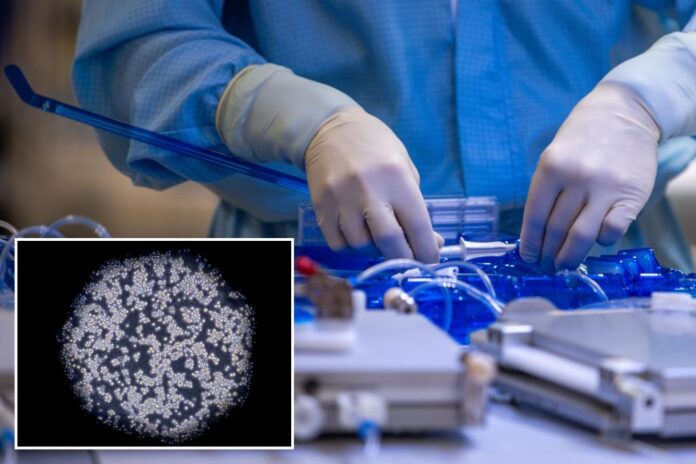
Scientists at the UC Davis Comprehensive Cancer Center in Sacramento, California, have identified a protein on the CD95 receptor that can “program” cancer cells to die, as detailed in a study published in the journal Cell Death & Differentiation last month.
A receptor is a protein within a cell that receives and transmits signals.
CD95 receptors — also referred to as Fas — have gained the nickname “death receptors” because they send a signal that causes cancer cells to “self-destruct,” according to a press release from UC Davis.
“Previous efforts to target this receptor have been unsuccessful. But now that we’ve identified this epitope (target), there could be a therapeutic path forward to target Fas in tumors,” Jogender Tushir-Singh, an associate professor in the Department of Medical Microbiology and Immunology and senior author of the study, said in the release.
Experts are hopeful that future cancer drugs could boost the activity of these CD95 receptors to create a new weapon against cancer tumors, which have been treated historically with surgery, chemotherapy and radiation.
Immune-based therapies, such as CAR (chimeric antigen receptor) T-cell therapy, have shown promise for a subset of patients, but have had limited effectiveness against many cancer types.

“Despite being decently successful in liquid tumors, such as leukemia spectrum cancers, long-term remission remains the biggest challenge for CAR T-cell therapies,” Tushir-Singh told Fox News Digital in an email.

The bigger challenge with this therapy — which typically costs $500,000 or more — is that it has only shown “meager success” in treating solid tumors, the researcher noted.
“Our study strongly provides a comprehensive takeaway and potential solution to transform the meager success of CAR-T therapies into potentially successful [therapies for] solid tumors.”
The newly discovered “kill switch” could terminate tumor cells while also helping to make immunotherapies more effective — “a potential one-two punch against tumors,” the release stated.
Thus far, no CD95-boosting drugs have made it into clinical trials.
“Despite many breakthroughs in the cancer immunotherapeutic field, targeting Fas remains neglected, primarily due to fear of retaliation against immune-system T-cells,” Tushir-Singh told Fox News Digital.
The study did have some limitations — namely, there is limited data from clinical trials, the researcher noted.
Tushir-Singh pointed out, however, that cancer researchers can now go back and collect human tumor samples from clinical trials and perform new analyses in light of these findings.
“It is evident that the success of CAR-T therapy relies on off-target killing by Fas,” he told Fox News Digital.
“With the current information, we researchers and doctors should screen potential cancer patients — who would be undergoing CAR-T therapy — to check for the comprehensive presence of Fas on their tumors,” he went on.
“If a patient lacks Fas expression in his or her tumors, we need to find ways to safely manipulate these tumors and start making them Fas before giving costly CAR therapies. The latter would likely make the CARs more potent in long-term efficacy.”
Looking ahead, Tushir-Singh said he is hopeful for the future of cancer treatments.
“Due to the advent of cancer immunotherapy and other targeted therapies, cancer rates overall in the past decades have decreased significantly,” he said.
“I read every day the outstanding research that is happening in the U.S. to beat cancer. People should stay positive.”
Added Tushir-Singh, “The next breakthrough is just one experiment away.”